Vaginitis: Symptoms, Causes & Treatment in Miami Gardens

If you’ve noticed itching, burning, unusual discharge, or a strong odor, you may have vaginitis. This simply means the tissue inside the vagina is irritated or inflamed. Vaginitis is common, and while it can be uncomfortable, it’s treatable.
At All-Inclusive Preventive Care in Miami Gardens, we understand that these symptoms can be stressful or even embarrassing. You deserve quick answers and relief. That’s why our bilingual team offers same-day appointments, evening and weekend hours, and on-site testing. Instead of waiting for hours in a hospital emergency room or sitting at an urgent care center, you can come straight to us for compassionate care.
📍 16361 NW 57th Ave, Miami Gardens, FL 33014
📞 (305) 200-3141
Gynecologist in Miami | Annual Gynecological Exam
What is vaginitis?
Vaginitis is inflammation (swelling and irritation) of the vagina or vulva. Normally, healthy bacteria called lactobacillus keep your vaginal pH (acid level) balanced. This balance protects you against infection.
When that balance is thrown off — for example by antibiotics, hormone changes during menopause, or an infection like trichomonas vaginalis (a tiny parasite passed through sex) — it can lead to odor, unusual discharge, or pain. Some patients don’t notice any symptoms (asymptomatic), but untreated vaginitis can still affect long-term health.
Symptoms you should watch for
Everyone’s experience is different, but these are the most common signs:
| Symptom | What it may mean | Why it matters |
|---|---|---|
| Unusual discharge (watery or “cottage cheese” thick) | Overgrowth of yeast or bacteria | Suggests a vaginal yeast infection or bacterial vaginosis (BV) |
| Strong, fishy odor | Often BV with higher pH | Linked to bacteria like Gardnerella vaginalis |
| Itching, burning, or skin irritation | Reaction to products (like soap, tampon, spermicide) or a fungus | Removing triggers and treating infection stops symptoms |
| Burning when passing urine (dysuria) | Irritation or infection | Needs the right medication |
| Pain during sex (dyspareunia) | Atrophic vaginitis from low estrogen or dryness | May need estradiol or other hormone therapy |
| Spotting or light vaginal bleeding | Infection, tissue atrophy, or irritation | Requires a physical examination |
| Pelvic pain or swelling (edema) | Infection spreading further | Should be checked quickly |
| Fever | Infection outside the vagina | May require emergency medicine |
If you’re pregnant: Vaginitis during pregnancy can raise the risk of preterm birth or low birth weight. Call your health care provider immediately if you have symptoms.
Causes of vaginitis
- Bacterial vaginosis (BV): Caused by too much growth of certain bacteria, such as Gardnerella vaginalis or Mycoplasma hominis.
- Yeast infection: An overgrowth of fungus (Candida). Often causes thick discharge, itch, and irritation.
- Trichomoniasis: A sexually transmitted infection caused by Trichomonas vaginalis. Spread through sexual intercourse or oral sex. May cause frothy discharge and strong odor.
- Other STIs: Infections such as chlamydia, gonorrhea, or herpes simplex virus can cause similar irritation. Some are asymptomatic - meaning that there are no noticeable symptoms so they are harder to detect without regular testing.
- Allergy or irritant(s): Reactions to fragranced toilet paper, tampons, feminine hygiene sprays, spermicide, harsh soap, or tight clothing/underwear.
- Atrophic vaginitis: Thinning of vaginal tissue (atrophy) linked to menopause, hypoestrogenism, or after childbirth/breastfeeding. Often causes dryness and dyspareunia.
- Risk factors: Disease or conditions like diabetes, HIV, immunodeficiency, prior surgery/scar, some forms of birth control (like an intrauterine device), and recent antibiotic use.
How vaginitis is diagnosed
At All-Inclusive Preventive Care, diagnosis begins with a review of your medical history and a pelvic exam. During the exam, your provider may gently use a cotton swab to collect a sample from the vagina and cervix. This process is quick and usually causes little to no discomfort.
Depending on your symptoms, tests may include:
- pH test: Checks the acid level inside the vagina. A higher pH can point to bacterial vaginosis (BV) or trichomonas.
- Saline wet mount: A sample is mixed with saline (salt water) and viewed under a microscope. This helps identify cells, yeast, or parasites like Trichomonas vaginalis.
- KOH prep: A solution called potassium hydroxide (KOH) is added to the sample. This makes fungus easier to see under the microscope and may release a “fishy” odor, which is a clue for BV.
- Polymerase chain reaction (PCR): An advanced nucleic acid test that looks for the DNA of infections such as chlamydia, gonorrhea, or trichomonas. PCR is very sensitive and can detect infections even in patients with no symptoms (asymptomatic).
These simple in-office tests help your provider find the exact cause of vaginitis so you get the right treatment and relief.
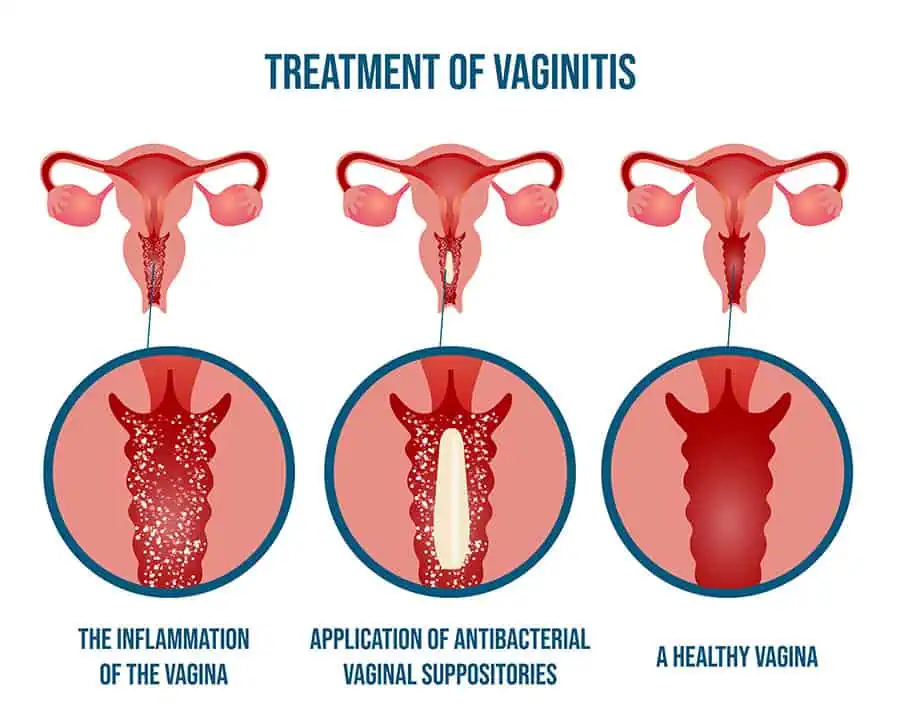
Treatment options
| Cause | Treatment | Medication | What patients should know |
|---|---|---|---|
| Bacterial vaginosis (BV) | Antibiotic | Metronidazole or Clindamycin | Take all doses; avoid alcohol with metronidazole |
| Yeast infection | Antifungal | Clotrimazole suppository or fluconazole | Add a probiotic (like yogurt with lactobacillus) to restore balance |
| Trichomoniasis | Antimicrobial | Oral metronidazole | Both partners must be treated; avoid sex until cleared |
| Atrophic vaginitis | Hormone therapy | Estradiol cream or vaginal ring | Restores moisture and reduces pain and discomfort during sex |
| Irritant/Allergic | Lifestyle changes | — | Avoid douche, harsh soap, spermicide, or perfumed feminine hygiene products |
Recovery tips
- Finish all medication. Stopping an antibiotic or antifungal early can make symptoms return.
- Rebuild balance. Add probiotics or lactobacillus supplements to support healthy vaginal flora.
- Treat partners if needed. With trichomonas, both partners must get treated. Always practice safe sex with a condom.
- Address menopause symptoms. For atrophic vaginitis, local hormone therapy like estradiol can improve dryness and comfort.
- Special cases. If you’re pregnant, have heavy bleeding, or ongoing pain, seek care quickly.
Prevention and self-care
You can lower your chances of vaginitis with a few daily habits:
- Practice safe sex. Use a condom and stay up to date with STI testing and cancer screening.
- Avoid harsh products. Don’t use a douche, fragranced soap, or perfumed feminine hygiene sprays.
- Choose breathable clothing. Wear cotton underwear and change after exercise or swimming.
- Support your immune system. A balanced diet, hydration, and regular exercise strengthen your body’s defenses.
- Pelvic floor care. Kegel exercises may help with dryness or dyspareunia.
- Stay proactive. Book your Annual Gynecological Exam or Annual Physical Exam in Miami.
When to seek care right away
Call your doctor or visit a clinic if you notice:
- Fever or pelvic pain
- Heavy vaginal bleeding
- Symptoms during pregnancy
- No improvement after OTC yeast infection treatment
- More than four infections in a year
- Painful sores, which may be herpes simplex virus
If severe, go to an urgent care center or hospital. For routine but concerning symptoms, schedule with our Miami Medical Clinic.
FAQs
Is vaginitis contagious?
It depends on the cause. Bacterial vaginosis (BV) and yeast infections usually come from changes in your own vaginal flora, so they aren’t considered contagious. Trichomonas vaginalis, however, is a sexually transmitted infection that spreads through sexual intercourse. In that case, both you and your partner will need treatment to prevent it from coming back.
How long does vaginitis last?
With the right medication, most patients feel better within 3–7 days. However, certain types like atrophic vaginitis (linked to menopause and low estrogen) can be ongoing and may need long-term hormone therapy for relief.
Can vaginitis cause cancer?
Not directly. Vaginitis itself does not turn into cancer. But if infections go untreated, they can make cancer screening more difficult or, in rare cases, increase the risk of cervical cancer. That’s why routine exams and early treatment are important.
Can vaginitis go away on its own?
Mild irritation sometimes improves with better hygiene or stopping products that cause irritation. But in most cases, vaginitis requires an antibiotic or antifungal medication to fully clear the infection and prevent symptoms from returning.
Vaginitis care in Miami Gardens
At All-Inclusive Preventive Care, our goal is simple: to help you feel better, faster. We provide accurate testing, clear answers, and compassionate therapy for vaginitis and related conditions. Beyond treatment, our women’s health team supports you with birth control, STI testing (including chlamydia, gonorrhea, and herpes), and routine preventive healthcare.
Our Miami Gardens clinic is designed for your convenience — with same-day appointments, bilingual staff, and evening hours so you don’t have to wait for relief. Whether you need answers about new symptoms or ongoing care to protect your long-term health, we’re here for you.
📞 Call (305) 200-3141 or book online today:
- Gynecologist in Miami
- Primary Care in Miami Gardens
- Annual Gynecological Exam
- Annual Physical Exam in Miami
This article was medically reviewed by Evelyn Rodriguez, APRN, owner at All-Inclusive Preventive Care in Miami Gardens, FL. Dr. Rodriguez completed her medical school residency in obstetrics and family planning and specializes in gynecology, preventive care, and sexual health services.
